Abstract
Introduction
Interim response evaluation by 18F-fluorodeoxyglucose (FDG) positron emission tomography (PET)/computed tomography (CT) (iPET) in diffuse large B cell lymphoma (DLBCL) is encouraged to rule out disease progression and has been suggested to be predictive of survival. However, treatment guidance by iPET is not yet recommended for DLBCL in clinical practice.
The aim of our study was to assess the predictive value of iPET in progression free survival (PFS) and overall survival (OS) in DLBCL patients (pts), interpreted according to visual and semiquantitative methods.
Methods
Single centre retrospective analysis of pts diagnosed with DLBCL from 2010 to 2019, uniformly treated with R-CHOP/R-CHOP-like protocols (6-8 cycles) and submitted to iPET assessment after 3-4 cycles of treatment, with no therapy change based on the latter. The iPET findings were interpreted using the visual Deauville 5-point scale (DS) and quantitative comparison of maximum standardized uptake value (SUVmax) before and during treatment. The percentage decrease in SUVmax between baseline PET (PET0) and iPET (ΔSUVmax) was calculated as follows: ΔSUVmax = (PET0 SUVmax-iPET SUVmax)/PET0 SUVmax × 100%. iPET with DS of 1-3 and ΔSUVmax ≥66% was defined as negative. Agreement between the 2 methods, DS and ΔSUVmax, was assessed by Cohen´s k computation. Cox regression model was used to estimate PFS and OS. Risk factors with p<0.1 in the univariate analysis were included in the multivariate model.
Results
A total of 335 pts were diagnosed with DLBCL. Forty-one percent (n=138) underwent iPET and SUVmax was available for 86 pts. Of these, 55.8% were male, with median age of 60 years old (24-84). At diagnosis, 72.1% presented with advanced stage disease, 55.8% with abnormal lactate dehydrogenase (LDH) and 49.4% with B symptoms. Bone marrow involvement and extranodal disease was present in 12% and 76.7%, respectively. According to International Prognostic Index (IPI) score, 44.7% of pts were intermediate-high/ high-risk.
At interim evaluation, 26.7% (n=23) had an iPET positive by DS, while 17.4% (n=15) had a ΔSUVmax <66%. Nine patients (10.5%) had an iPET positive by DS and ΔSUVmax <66%. A fair agreement between DS and ΔSUVmax was observed (k=0.333).
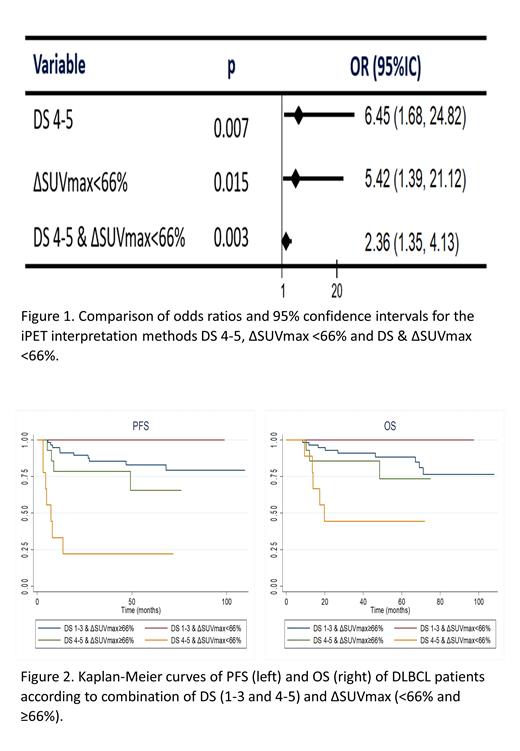
Primary refractoriness (PrR) and/or disease progression, defined according to Lugano criteria, was seen in 22.1% of the pts. iPET positivity, measured either by DS (OR 6.45 [95%CI: 1.68-24.82], p=0.007) or ΔSUVmax (OR 5.42, [95%CI: 1.39-21.12], p=0.015), showed predictive value of PrR, improved by combining the DS and the ΔSUVmax in iPET interpretation (OR 2.36 [95%CI: 1.35-4.13], p=0.003) (Figure 1).
For a median follow-up of 50.1 months, median PFS was not reached (NR) and was higher in iPET negative pts, regardless of the interpretation by DS (84.3% versus 49.0% at 5 years; HR 4.27, p<0.001) or ΔSUVmax ≥66% (91.5% versus 60.4% at 5 years; HR 3.63, p=0.003). The impact of iPET negativity when assessed by DS became not significant after multivariate analysis (HR 2.86, p=0.07), however remained predictive of PFS when interpreted by ΔSUVmax ≥66% (HR 3.53, p=0.02).
Median OS was NR and was higher in the iPET negative group, when assessed by DS (89.3% versus 62.2% at 5 years, HR 3.49, p=0.01). By contrast, ΔSUVmax ≥66% did not prove to be predictive of OS (85.8% versus 65.7% at 5 years, HR 2.63, p=0.06). The impact of iPET negativity on OS was not significant upon multivariate analysis, regardless scan measurement by DS or ΔSUVmax ≥66% (HR 4.01, p=0.07 for DS, and HR 1.06, p=0.94, for ΔSUVmax ≥66%).
Interestingly, combined visual and semiquantitative analysis allowed to identify a very high-risk subgroup of patients in our cohort, with significantly inferior PFS and OS (PFS: HR 9.60, p<0.001, 81.3% vs 22.2% at 5 years; OS: HR 5.20, p<0.001, 86.7% vs 44.4% at 5 years) (Figure 2).
Conclusion
Our results showed that, in our cohort, ΔSUVmax semiquantitative method in iPET interpretation has an independent predictive value of PFS, but not of OS. iPET sub-analysis with combined DS and ΔSUVmax allowed to identify a very high-risk group of DLBCL pts with markedly inferior PFS and OS. In addition, both DS and ΔSUVmax are good predictors of primary refractoriness, particularly when both visual and semiquantitative methods are combined.
Gomes: Takeda: Consultancy; Gilead: Consultancy; Janssen: Consultancy.